The Japan cannabis use disorder treatment demand is valued at USD 83.7 million in 2025 and is forecasted to reach USD 118.4 million by 2035, reflecting a CAGR of 3.5%. Demand is influenced by increased identification of substance-use disorders, expansion of psychiatric screening programmes, and wider recognition of cannabis-related dependence as a public health concern. Rising utilization of structured therapy pathways, integration of addiction services within mental-health systems, and continued policy attention toward early intervention support stable treatment uptake across clinical settings. Clinical interventions for marijuana-related dependence account for the largest share. Treatment centers rely on cognitive behavioural therapy, motivational enhancement strategies, relapse-prevention frameworks, and rehabilitation support designed for long-term behavioural management. These approaches remain central as Japan maintains strict regulations on cannabis use and prioritizes non-pharmacological treatment pathways for affected individuals.
Kyushu & Okinawa, Kanto, and Kansai register the highest utilization levels due to their extensive hospital networks, specialized psychiatric facilities, and established mental-health support infrastructure. These regions also host community-based rehabilitation programmes and counselling services that strengthen treatment accessibility. Key organizations include the National Center of Neurology and Psychiatry (NCNP), Japan Alcohol and Drug Addiction Rehabilitation Center (DARC Network), Japanese Society of Psychiatry and Neurology (JSPN), Prefectural Mental Health and Welfare Centers, and private psychiatric hospitals and addiction clinics. These institutions provide assessment, counselling, rehabilitation, and long-term support for individuals with cannabis use disorder.
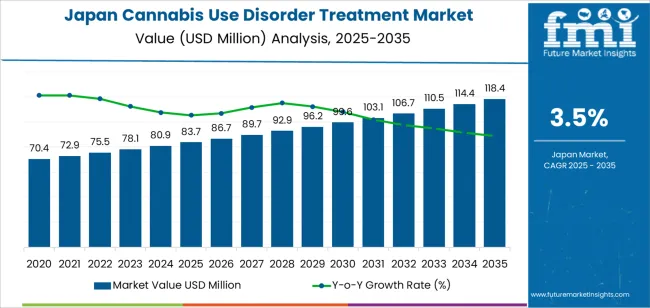
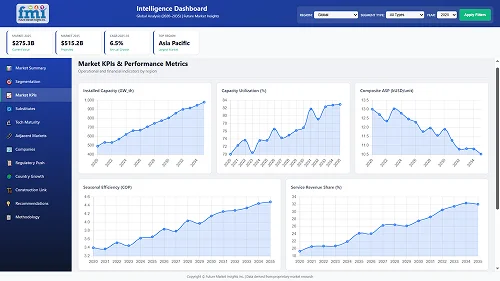
Growth rate volatility in Japan’s cannabis-use-disorder treatment segment remains low because demand is shaped primarily by regulatory structures, limited prevalence, and controlled clinical pathways. Annual variation is narrow in the early period as treatment access is tied to specialist care settings, where patient volumes change slowly and referral patterns remain stable. Public-health programmes and mental-health services follow fixed protocols, which reinforces predictable utilization.
Mid-period volatility remains limited because the segment expands within a tightly regulated environment. Awareness initiatives, clinician training, and incremental development of structured treatment frameworks contribute to steady but modest increases. Since cannabis use in Japan remains low by international comparison, shifts in patient numbers tend to be gradual, preventing sharp year-to-year swings. Institutional adoption of treatment models also progresses at a controlled pace due to strict compliance expectations.
Late-period volatility stays contained as treatment services mature and follow established behavioural-health processes. Growth depends mainly on incremental increases in screening, early-intervention programmes, and integration with broader addiction-care systems. These changes move slowly and keep volatility compressed.
| Metric | Value |
|---|---|
| Japan Cannabis Use Disorder Treatment Sales Value (2025) | USD 83.7 million |
| Japan Cannabis Use Disorder Treatment Forecast Value (2035) | USD 118.4 million |
| Japan Cannabis Use Disorder Treatment Forecast CAGR (2025-2035) | 3.5% |
Demand for cannabis use disorder treatment in Japan is increasing because healthcare providers and public health agencies are observing gradual growth in cases linked to recreational experimentation, illicit product availability and rising awareness of dependency risks. Although overall cannabis use remains low compared with many countries, enforcement data and clinical reports show more individuals experiencing psychological dependence, withdrawal symptoms and social or occupational challenges that require structured intervention. Hospitals and mental health clinics integrate screening tools into psychiatric and addiction services, which increases detection.
Educational campaigns encourage families to seek early clinical support, strengthening demand for counselling, behavioural therapy and relapse-prevention programmes. Universities and community centers also promote awareness of substance-related risks, prompting more referrals to treatment facilities. Constraints include limited number of specialized addiction-treatment programmes for cannabis specifically, social stigma that discourages early help-seeking, and lack of broad public understanding of cannabis-related mental health symptoms. Regulatory restrictions on research and treatment innovation also slow expansion of evidence-based approaches. Some individuals avoid formal services due to concerns about legal consequences or privacy.
Demand for cannabis use disorder treatment in Japan reflects increasing clinical attention to substance-related behavioral concerns across young adults, working-age groups, and individuals with concurrent mental health needs. Treatment programs vary by substance type, severity of dependence, and patterns of polydrug use involving marijuana, alcohol, tobacco, and synthetic cannabinoids. Facilities offering care range from hospitals to rehabilitation centers, shaped by Japan’s structured healthcare system and preference for supervised interventions. The treatment mix includes counseling-based programs, detoxification support, and medication-assisted therapy for associated symptoms. This pattern shows how Japan addresses cannabis-related disorders within broader substance use frameworks, focusing structured environments, psychological support, and coordinated follow-up care.
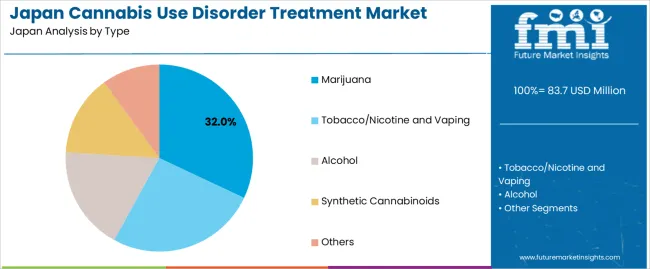
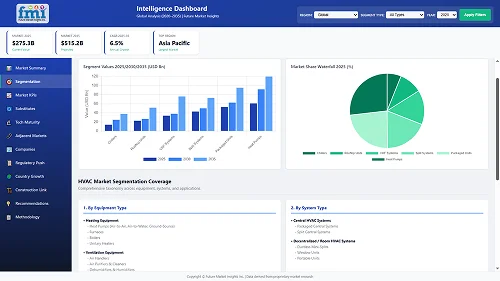
Marijuana accounts for 32.0% of treatment demand and remains the leading substance category for cannabis use disorder interventions in Japan. Increased exposure to imported cannabis products and illegal THC-containing items contributes to treatment entry within younger groups. Tobacco, nicotine, and vaping products represent 26.0%, reflecting overlapping dependence patterns identified during clinical assessments. Alcohol accounts for 18.0%, often appearing in co-occurring substance use cases requiring integrated support. Synthetic cannabinoids hold 14.0%, linked to adverse psychological effects that require monitored intervention. Other substances represent 10.0%, covering mixed or unclear-use cases. Distribution across substances shows how treatment professionals manage diverse dependence triggers and behavioral patterns.
Key points:
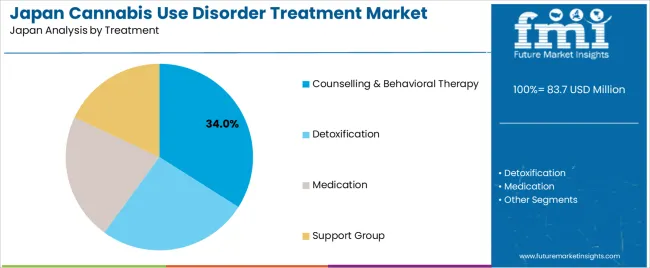
Counselling and behavioral therapy accounts for 34.0% and remains Japan’s most used intervention for cannabis use disorder. These programs emphasize structured guidance, relapse prevention, and coping strategies suited to varying dependence levels. Detoxification represents 26.0%, applied when withdrawal symptoms or co-occurring use patterns require medical supervision. Medication accounts for 22.0%, focusing on associated anxiety, sleep disturbance, or comorbid mental health concerns. Support groups represent 18.0%, reflecting participation in peer-led programs that complement formal therapy. Treatment distribution shows how Japan applies a blended care model combining psychological support, supervised detox, and symptom-targeted pharmacologic strategies managed through regulated providers.
Key points:
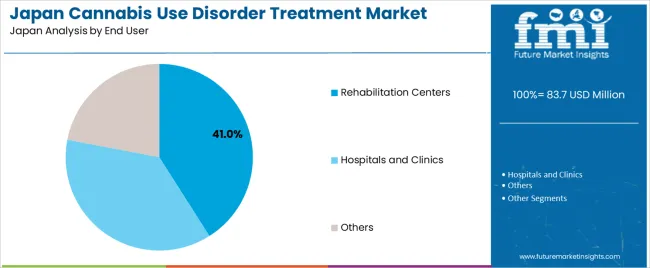
Rehabilitation centers account for 41.0% and serve as Japan’s primary settings for cannabis use disorder treatment. These facilities provide structured programs, predictable routines, and monitored interventions suited to medium- and long-term recovery. Hospitals and clinics represent 37.0%, focusing on diagnosis, early-stage intervention, and cases requiring medical oversight. Other end users account for 22.0%, including counseling offices, community programs, and private support facilities offering varied engagement levels. End-user distribution reflects Japan’s focus on supervised, clinically guided environments supported by standardized assessment protocols and formal treatment pathways designed to manage dependence severity and prevent relapse.
Key points:
Increased detection of cannabis-related offenses, rising referrals through the criminal justice system and expansion of prefectural addiction-consultation services are driving demand.
In Japan, demand for cannabis use disorder treatment is shaped by strict enforcement of the Cannabis Control Act, which leads police and regional prosecutors to refer offenders to medical and counselling services rather than rely solely on penal measures. Prefectures such as Tokyo, Osaka and Kanagawa have reported gradual increases in cannabis-related arrests among younger adults, prompting more evaluations at mental-health clinics. Public addiction-consultation centers operated by local governments provide free early-stage counselling, which increases treatment access for individuals identified through school, workplace or family interventions. These structural pathways contribute to steady demand for professional support services.
Strong social stigma, limited specialized treatment programs and reluctance among users to engage in clinical support restrain adoption.
Japan’s strict cultural norms around drug use create significant stigma, discouraging individuals from seeking help until legal involvement forces assessment. Few medical institutions offer specialized cannabis-focused treatment programs, and most substance-use services prioritize alcohol dependence, resulting in limited tailored interventions. Families may avoid contacting addiction services due to concerns about social consequences, reducing early engagement. These behavioural and systemic factors restrict treatment volume despite government efforts to promote early consultation.
Expansion of youth-focused prevention programs, increased involvement of psychiatric clinics and growth of confidential tele-counselling services define key trends.
Education boards in prefectures such as Tokyo, Saitama and Fukuoka are expanding drug-awareness programs targeting high school and university students, which increases early referrals for counselling. Psychiatric clinics are incorporating structured behavioural therapy and relapse-prevention tools tailored to younger adults who represent a growing share of cannabis cases. Tele-counselling platforms operated by local governments and nonprofit organizations provide confidential access to consultation, which reduces stigma-related barriers and encourages individuals to seek guidance without visiting clinics. These trends indicate slow but increasing institutional capacity for cannabis use disorder treatment within Japan.
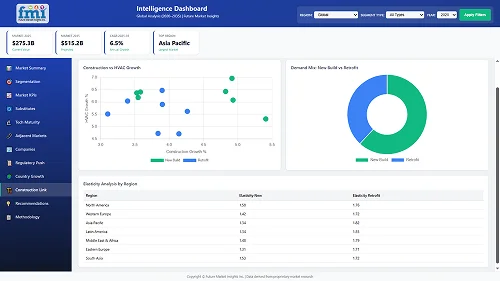
Demand for cannabis use disorder treatment in Japan is increasing through 2035 as healthcare providers, mental-health institutions, public-health agencies, and counseling services expand structured programs addressing substance-use behaviors. Treatment demand is shaped by regional healthcare capacity, awareness programs, and the gradual increase in individuals seeking behavioral-health support. Services typically include psychological counseling, outpatient interventions, cognitive-behavioral approaches, and coordinated care between hospitals and community clinics. Kyushu & Okinawa leads at 4.4%, followed by Kanto (4.1%), Kansai (3.6%), Chubu (3.1%), Tohoku (2.7%), and Rest of Japan (2.6%).
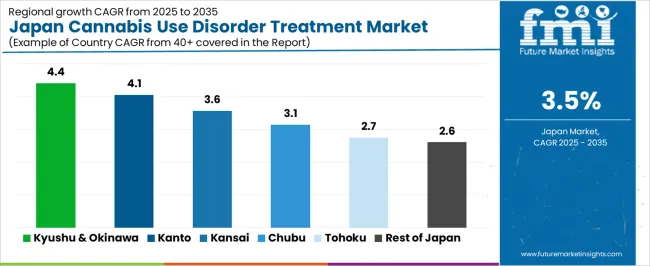
| Region | CAGR (2025-2035) |
|---|---|
| Kyushu & Okinawa | 4.4% |
| Kanto | 4.1% |
| Kansai | 3.6% |
| Chubu | 3.1% |
| Tohoku | 2.7% |
| Rest of Japan | 2.6% |
Kyushu & Okinawa grows at 4.4% CAGR, supported by active regional health networks, rising patient engagement with mental-health services, and broad outreach programs conducted by municipal health offices. Prefectures such as Fukuoka, Kagoshima, and Kumamoto maintain structured addiction-treatment pathways involving psychiatric clinics, hospital outpatient units, and community counseling centers. Okinawa reports additional demand due to its younger demographic groups and strong presence of community-based support organizations, leading to higher screening participation. Public-health programs emphasize early intervention, encouraging individuals to seek behavioral guidance before symptoms escalate. Healthcare providers collaborate with local schools, welfare offices, and community programs to identify cases requiring structured counseling.
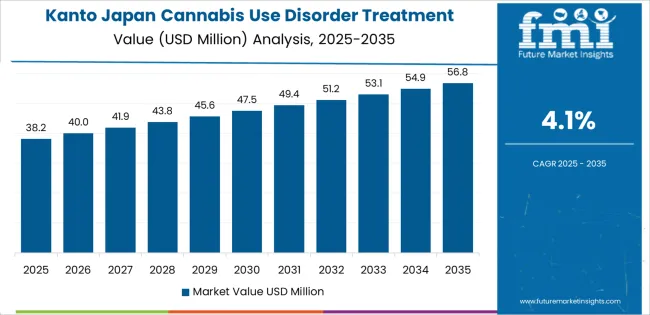
Kanto grows at 4.1% CAGR, influenced by high population density, extensive healthcare infrastructure, and strong integration of mental-health services across Tokyo, Kanagawa, Saitama, and Chiba. Urban clinics and psychiatric departments deliver structured therapy programs focused on behavioral modification and relapse-prevention strategies. Public-health centers conduct awareness campaigns focusing early consultation and confidential treatment access. Colleges and vocational schools in the region partner with mental-health professionals to support screening initiatives for young adults. Municipal welfare offices coordinate referrals to counseling specialists for long-term follow-up. Healthcare institutions in Tokyo maintain multidisciplinary teams that support case management and tailored intervention schedules.
Kansai grows at 3.6% CAGR, supported by established psychiatric-care networks, university communities, and municipal programs in Osaka, Kyoto, and Kobe. Healthcare providers offer counseling, behavioral-health evaluation, and continuing care for individuals seeking structured support. Student populations in Kyoto and Osaka create additional engagement with campus-linked counseling centers, which often serve as early points of contact. Local governments run awareness programs encouraging voluntary consultations. Hospitals in Osaka and Kobe maintain specialized outpatient mental-health units capable of providing long-term follow-up and coordinated psychotherapy. Community centers host informational workshops that address behavioral-health management and encourage early intervention.
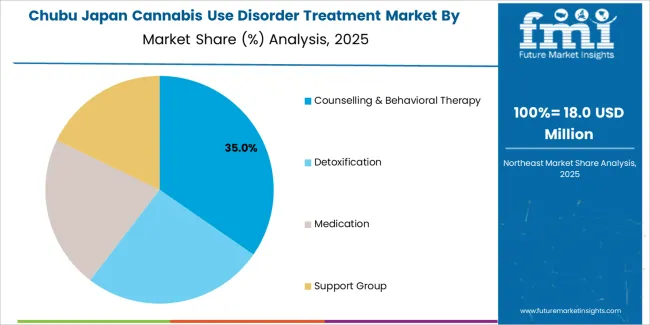
Chubu grows at 3.1% CAGR, shaped by balanced urban-rural healthcare networks, consistent use of mental-health resources, and structured community-health programs across Nagoya, Shizuoka, and nearby prefectures. Psychiatric clinics offer therapy sessions focused on behavioral-adjustment support. Hospitals maintain outpatient mental-health departments that assist with structured treatment pathways. Municipal health offices conduct workshops encouraging early identification. Supervised counseling services are offered through welfare centers for individuals seeking confidential behavioral-health guidance. Distribution of informational materials through schools and community groups helps maintain awareness.
Tohoku grows at 2.7% CAGR, supported by regional healthcare networks, public-health initiatives, and reliance on community-level support services across Sendai, Akita, Aomori, and Fukushima. Households rely on local clinics for mental-health consultations, while hospitals provide structured outpatient treatment. Public-health centers integrate substance-use awareness programs into community events, promoting access to counseling. Rural areas depend on municipal welfare offices and tele-health channels for early behavioral-health evaluation. Educational institutions participate in preventive-education efforts targeting young populations.
Rest of Japan grows at 2.6% CAGR, influenced by smaller population clusters, moderate availability of mental-health resources, and reliance on community-based interventions. Local clinics provide basic counseling and referral pathways to larger regional hospitals. Households access public-health consultations during community events, where screening and informational materials are distributed. Municipal offices coordinate support for individuals seeking long-term behavioral-health management. Schools and local welfare groups participate in preventive education to increase early awareness. Tele-health services support access in remote areas, ensuring continuity of care despite limited specialist availability.
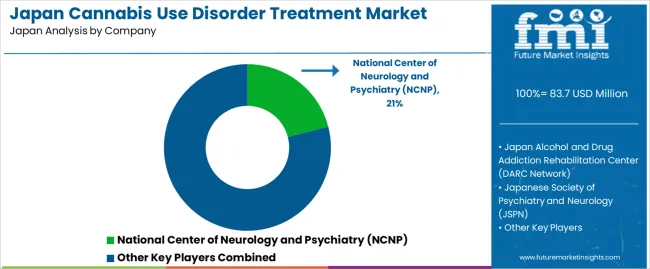
Demand for cannabis use disorder treatment in Japan is shaped by public institutions, psychiatric centers, and nationwide rehabilitation networks rather than pharmaceutical suppliers. The National Center of Neurology and Psychiatry (NCNP) holds an estimated 21.0% share of structured treatment activity through its Center for Dependence Disorders. The organization provides controlled psychological assessment, behavioural-therapy programmes, and evidence-based interventions aligned with national mental-health protocols.
The DARC Network maintains extensive coverage across prefectures, supporting individuals through residential and community-based rehabilitation programmes. These centers provide consistent counselling frameworks, peer-support environments, and relapse-prevention training, forming a core part of Japan’s non-medical treatment ecosystem. The Japanese Society of Psychiatry and Neurology (JSPN) contributes through clinical guidelines and practitioner support within hospitals and psychiatric clinics, ensuring a uniform approach to assessment and treatment of substance-use disorders, including cannabis use.
Prefectural Mental Health and Welfare Centers play a major role in early intervention, providing accessible counselling and case-management services for individuals referred through schools, families, or law-enforcement channels. Private psychiatric hospitals and addiction clinics add further capacity through structured outpatient treatment and cognitive-behavioural programmes adapted to individual clinical needs. Competition within Japan centers on clinical capacity, regional accessibility, therapeutic consistency, counselling quality, and coordination with public-health frameworks. Demand for treatment is shaped by strict legal enforcement, rising early-intervention initiatives, and increased counselling utilization, reinforcing the central role of public institutions and rehabilitation networks in managing cannabis use disorder within the country.
| Items | Values |
|---|---|
| Quantitative Units | USD million |
| Type | Marijuana, Tobacco/Nicotine and Vaping, Alcohol, Synthetic Cannabinoids, Others |
| Treatment | Counselling & Behavioral Therapy, Detoxification, Medication, Support Group |
| End User | Rehabilitation Centers, Hospitals and Clinics, Others |
| Regions Covered | Kyushu & Okinawa, Kanto, Kansai, Chubu, Tohoku, Rest of Japan |
| Key Companies Profiled | National Center of Neurology and Psychiatry (NCNP), Japan Alcohol and Drug Addiction Rehabilitation Center (DARC Network), Japanese Society of Psychiatry and Neurology (JSPN), Prefectural Mental Health and Welfare Centers, Private psychiatric hospitals and addiction clinics |
| Additional Attributes | Dollar spending by treatment type, substance category, and end-user group; regional adoption trends across Kyushu & Okinawa, Kanto, Kansai, Chubu, Tohoku, and Rest of Japan; influence of Japan’s strict drug regulations on treatment uptake; growth of structured rehabilitation programs, outpatient addiction services, and cognitive behavioral therapy; monitoring systems for cannabis-related psychiatric cases; role of government-supported mental health centers and private addiction clinics in expanding treatment access. |
The demand for cannabis use disorder treatment in Japan is estimated to be valued at USD 83.7 million in 2025.
The market size for the cannabis use disorder treatment in Japan is projected to reach USD 118.4 million by 2035.
The demand for cannabis use disorder treatment in Japan is expected to grow at a 3.5% CAGR between 2025 and 2035.
The key product types in cannabis use disorder treatment in Japan are marijuana, tobacco/nicotine and vaping, alcohol, synthetic cannabinoids and others.
In terms of treatment, counselling & behavioral therapy segment is expected to command 34.0% share in the cannabis use disorder treatment in Japan in 2025.
Our Research Products

The "Full Research Suite" delivers actionable market intel, deep dives on markets or technologies, so clients act faster, cut risk, and unlock growth.

The Leaderboard benchmarks and ranks top vendors, classifying them as Established Leaders, Leading Challengers, or Disruptors & Challengers.

Locates where complements amplify value and substitutes erode it, forecasting net impact by horizon

We deliver granular, decision-grade intel: market sizing, 5-year forecasts, pricing, adoption, usage, revenue, and operational KPIs—plus competitor tracking, regulation, and value chains—across 60 countries broadly.

Spot the shifts before they hit your P&L. We track inflection points, adoption curves, pricing moves, and ecosystem plays to show where demand is heading, why it is changing, and what to do next across high-growth markets and disruptive tech

Real-time reads of user behavior. We track shifting priorities, perceptions of today’s and next-gen services, and provider experience, then pace how fast tech moves from trial to adoption, blending buyer, consumer, and channel inputs with social signals (#WhySwitch, #UX).

Partner with our analyst team to build a custom report designed around your business priorities. From analysing market trends to assessing competitors or crafting bespoke datasets, we tailor insights to your needs.
Supplier Intelligence
Discovery & Profiling
Capacity & Footprint
Performance & Risk
Compliance & Governance
Commercial Readiness
Who Supplies Whom
Scorecards & Shortlists
Playbooks & Docs
Category Intelligence
Definition & Scope
Demand & Use Cases
Cost Drivers
Market Structure
Supply Chain Map
Trade & Policy
Operating Norms
Deliverables
Buyer Intelligence
Account Basics
Spend & Scope
Procurement Model
Vendor Requirements
Terms & Policies
Entry Strategy
Pain Points & Triggers
Outputs
Pricing Analysis
Benchmarks
Trends
Should-Cost
Indexation
Landed Cost
Commercial Terms
Deliverables
Brand Analysis
Positioning & Value Prop
Share & Presence
Customer Evidence
Go-to-Market
Digital & Reputation
Compliance & Trust
KPIs & Gaps
Outputs
Full Research Suite comprises of:
Market outlook & trends analysis
Interviews & case studies
Strategic recommendations
Vendor profiles & capabilities analysis
5-year forecasts
8 regions and 60+ country-level data splits
Market segment data splits
12 months of continuous data updates
DELIVERED AS:
PDF EXCEL ONLINE
Cannabis Use Disorder Treatment Market – Trends & Innovations 2025 to 2035
Opioid Use Disorder Treatment Industry Analysis by Opioid Antagonists and Opioid Agonists and Partial Agonists through 2035
Market Positioning & Share in the Opioid Use Disorder Treatment Sector
Alcohol Use Disorder Treatment Market Growth - Demand & Innovations 2025 to 2035
Substance Use Disorder Treatment Market Size and Share Forecast Outlook 2025 to 2035
Market Share Distribution Among Opioid Use Disorder Treatment Providers in Europe
Australia & NZ Opioid Use Disorder Treatment Market Analysis – Size, Share & Forecast 2025-2035
Menopause Treatment Industry Analysis in India Forecast Outlook 2025 to 2035
Menopause Treatment Market Analysis - Size, Share, and Forecast Outlook 2025 to 2035
Japan Axillary Hyperhidrosis Treatment Market Insights – Size, Share & Trends 2025-2035
Bipolar Disorder Drugs and Treatment Market Overview – Trends & Forecast 2025 to 2035
Japan Biliary Tract Cancers (BTCs) Treatment Market Growth – Demand, Trends & Forecast 2025-2035
Frontotemporal Disorders Treatment Market Size and Share Forecast Outlook 2025 to 2035
Anxiety Disorders And Depression Treatment Market Size and Share Forecast Outlook 2025 to 2035
Demand for Burns Treatment in Japan Size and Share Forecast Outlook 2025 to 2035
Major Depressive Disorder (MDD) Treatment Market Analysis – Growth & Forecast 2025 to 2035
Generalized Anxiety Disorder Treatment Market Insights by Drug Class, Therapies, Distribution Channel, and Region 2035
Lymphoproliferative Disorder Treatment Market
Demand for Hydrogen Buses in Japan Size and Share Forecast Outlook 2025 to 2035
Demand for Cannabis Packaging Equipment in Japan Size and Share Forecast Outlook 2025 to 2035
Thank you!
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.
Chat With
MaRIA