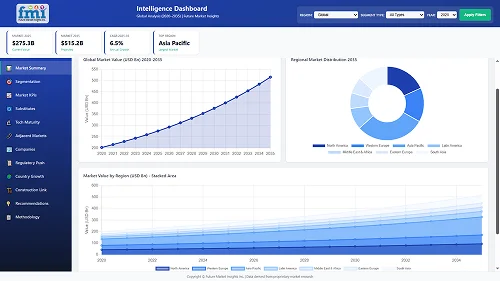
The third-party administration service market is projected to grow from USD 9.6 billion in 2025 to USD 14.1 billion by 2035 at a 3.9% CAGR during the forecast period, owing to steady expansion supported by rising outsourcing of healthcare and insurance administrative functions. In the first half of the forecast period, the market is expected to reach approximately USD 11.6 billion by 2030, adding USD 2.0 billion and accounting for 44% of total projected growth. This phase is influenced by the increasing adoption of employee benefits administration platforms as organizations streamline human resource operations and reduce internal administrative workload. Healthcare providers and insurers are prioritizing TPA partnerships to improve cost visibility, enhance claims accuracy, and accelerate reimbursement cycles. The growing complexity of benefit design structures and compliance management requirements across global employee programs also supports this trend.
In the second half of the period, demand will be shaped by the integration of digital claims adjudication tools, predictive analytics, and automated document processing systems. TPAs offering scalable data platforms, real-time reporting dashboards, and customizable service models are expected to gain stronger competitive positioning. Expansion of private health insurance participation in emerging economies and rising corporate focus on cost-efficient employee health management will further reinforce market momentum. Remote and hybrid workforce patterns are driving organizations to seek centralized and standardized benefits administration frameworks, creating sustained demand for professional TPA service providers across corporate, healthcare, and insurance ecosystems.
-service-market-market-value-analysis.webp)
The latter half (2030-2035) will witness sustained growth from USD 11.6 billion to USD 14.1 billion, representing an addition of USD 2.5 billion or 56% of the decade's expansion. This period will be defined by mass market penetration of specialized administrative designs, integration with comprehensive healthcare platforms, and seamless compatibility with existing insurance infrastructure. The market trajectory signals fundamental shifts in how organizations approach benefit optimization and claims quality management, with participants positioned to benefit from sustained demand across multiple service types and end-use industry segments.
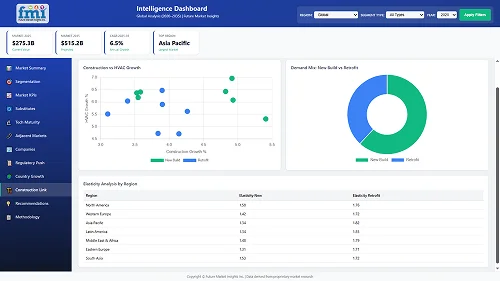
The Third Party Administration (TPA) Service market demonstrates distinct growth phases with varying market characteristics and competitive dynamics. Between 2025 and 2030, the market progresses through its technology adoption phase, expanding from USD 9.6 billion to USD 11.6 billion with steady annual increments averaging 3.9% growth. This period showcases the transition from basic administrative services to advanced employee benefits TPA systems with enhanced processing capabilities and integrated quality control systems becoming mainstream features.
The 2025-2030 phase adds USD 2.0 billion to market value, representing 44% of total decade expansion. Market maturation factors include standardization of benefits administration and healthcare industry protocols, declining technology costs for specialized administrative platforms, and increasing industry awareness of outsourcing benefits reaching 95-98% processing efficiency in healthcare and insurance applications. Competitive landscape evolution during this period features established TPA providers like Public Consulting Group and Andesa expanding their service portfolios while specialty administrators focus on advanced technology development and enhanced compliance capabilities.
From 2030 to 2035, market dynamics shift toward advanced platform integration and global service expansion, with growth continuing from USD 11.6 billion to USD 14.1 billion, adding USD 2.5 billion or 56% of total expansion. This phase transition centers on specialized administrative systems, integration with automated healthcare networks, and deployment across diverse insurance and benefits scenarios, becoming standard rather than specialized applications. The competitive environment matures with focus shifting from basic processing capability to comprehensive benefit optimization systems and integration with compliance monitoring platforms.
| Metric | Value |
|---|---|
| Market Value (2025) | USD 9.6 billion |
| Market Forecast (2035) | USD 14.1 billion |
| Growth Rate | 3.9% CAGR |
| Leading Technology | Employee Benefits TPA Service Type |
| Primary Application | Healthcare Industry Application Segment |
The market demonstrates strong fundamentals with employee benefits TPA systems capturing a dominant share through advanced administrative design and processing optimization capabilities. Healthcare industry applications drive primary demand, supported by increasing corporate outsourcing and cost-effective administrative technology requirements. Geographic expansion remains concentrated in developed markets with established insurance infrastructure, while emerging economies show accelerating adoption rates driven by healthcare expansion and rising regulatory standards.
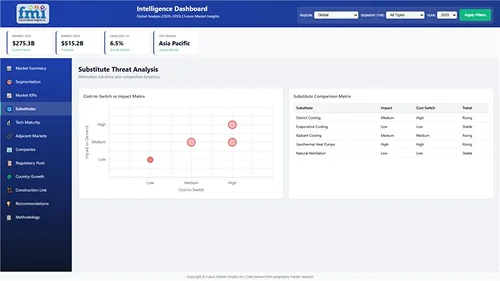
Market expansion rests on three fundamental shifts driving adoption across the healthcare, insurance, and corporate sectors. First, administrative cost reduction creates compelling operational advantages through TPA services that provide immediate processing efficiency and claims management without compromising service quality, enabling organizations to meet stringent regulatory standards while maintaining operational productivity and reducing overhead expenses. Second, healthcare administration modernization accelerates as insurance carriers worldwide seek advanced TPA systems that complement traditional processing methods, enabling precise benefit customization and compliance control that align with industry standards and regulatory requirements.
Third, employee benefit enhancement drives adoption from corporate employers and insurance providers requiring effective administrative solutions that maximize benefit value while maintaining operational productivity during enrollment and claims operations. However, growth faces headwinds from data security cost challenges that vary across TPA providers regarding the protection of sensitive health information and financial data, which may limit adoption in highly regulated environments. Technical limitations also persist regarding system integration concerns and legacy platform compatibility that may reduce effectiveness in complex multi-carrier scenarios, which affect processing performance and operational requirements.
The third party administration service market represents a specialized yet critical outsourcing opportunity driven by expanding global healthcare complexity, insurance modernization, and the need for superior administrative efficiency in diverse benefit applications. As organizations worldwide seek to achieve 95-98% processing accuracy, reduce administrative costs, and integrate advanced TPA systems with automated platforms, third party administration services are evolving from basic processing functions to sophisticated management solutions ensuring compliance and operational leadership.
The market's growth trajectory from USD 9.6 billion in 2025 to USD 14.1 billion by 2035 at a 3.9% CAGR reflects fundamental shifts in healthcare industry outsourcing requirements and administrative cost optimization. Geographic expansion opportunities are particularly pronounced in Asia Pacific markets, while the dominance of employee benefits TPA systems and healthcare industry applications provides clear strategic focus areas.
Strengthening the dominant employee benefits TPA segment through enhanced administrative capabilities, superior compliance performance, and automated processing systems. This pathway focuses on optimizing service delivery, improving enrollment efficiency, extending operational effectiveness to 95-98% accuracy rates, and developing specialized solutions for diverse applications. Market leadership consolidation through advanced technology integration and automated platform development enables premium positioning while defending competitive advantages against internal administration alternatives. Expected revenue pool: USD 180-240 million
Rapid healthcare and insurance industry growth across Asia Pacific creates substantial expansion opportunities through local service capabilities and technology transfer partnerships. Growing corporate benefits programs and government healthcare initiatives drive sustained demand for advanced TPA systems. Localization strategies reduce service costs, enable faster regulatory support, and position companies advantageously for corporate procurement programs while accessing growing domestic markets. Expected revenue pool: USD 150-200 million
Expansion within the dominant healthcare industry segment (40.0% market share) through specialized TPA services addressing medical claims standards and high-volume processing requirements. This pathway encompasses automated claims systems, regulatory compliance integration, and compatibility with diverse healthcare provider processes. Premium positioning reflects superior processing accuracy and comprehensive regulatory compliance supporting modern healthcare administration. Expected revenue pool: USD 130-175 million
Strategic expansion into insurance industry applications (35.0% market share) requires enhanced processing capabilities and specialized administrative solutions addressing carrier operational requirements. This pathway addresses multi-carrier management, policy administration enhancement, and claims adjudication services with advanced technology engineering for demanding regulatory standards. Premium pricing reflects specialized compliance requirements and extended processing standards. Expected revenue pool: USD 110-150 million
Expansion of healthcare TPA segment through medical claims expertise, provider network management, and specialized healthcare administration requiring comprehensive industry knowledge. This pathway encompasses utilization management, medical bill review, and care coordination services for complex healthcare applications. Market development through healthcare expertise enables differentiated positioning while accessing specialized markets requiring medical administration solutions. Expected revenue pool: USD 95-130 million
Development of specialized administrative services for pension TPA and risk management TPA segments, addressing specific retirement plan requirements and workers' compensation administration demands. This pathway encompasses retirement plan administration, ERISA compliance, and occupational injury management with proprietary technology solutions. Technology differentiation through specialized platforms enables diversified revenue streams while reducing dependency on single service categories. Expected revenue pool: USD 85-115 million
Development of superior compliance administrative solutions addressing regulatory requirements and data security standards across healthcare and insurance applications. This pathway encompasses HIPAA compliance integration, cybersecurity protocols, and comprehensive regulatory documentation. Premium positioning reflects compliance leadership and technology expertise while enabling access to highly regulated procurement programs and security-focused corporate partnerships. Expected revenue pool: USD 70-95 million
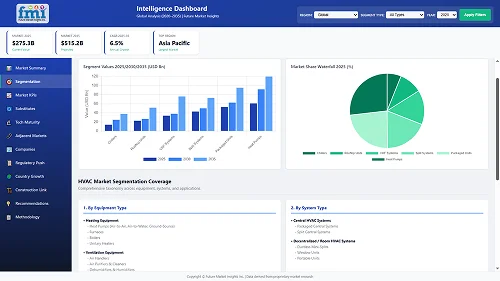
Primary Classification: The market segments by service type into Employee Benefits TPA, Healthcare TPA, Pension TPA, Risk Management TPA, and Others categories, representing the evolution from basic administrative services to specialized management solutions for comprehensive benefit optimization.
Secondary Classification: Application segmentation divides the market into Healthcare Industry, Insurance Industry, Construction and Real Estate Industry, Transportation Industry, and Others sectors, reflecting distinct requirements for administrative complexity, processing capacity, and regulatory compliance standards.
Regional Classification: Geographic distribution covers Asia Pacific, Europe, North America, and other regions, with developed markets leading adoption while emerging economies show accelerating growth patterns driven by healthcare expansion programs.
The segmentation structure reveals technology progression from standard administrative platforms toward specialized service systems with enhanced compliance and processing capabilities, while application diversity spans from healthcare claims processing to specialized pension and risk management applications requiring precise administrative solutions.
-service-market-analysis-by-service-type.webp)
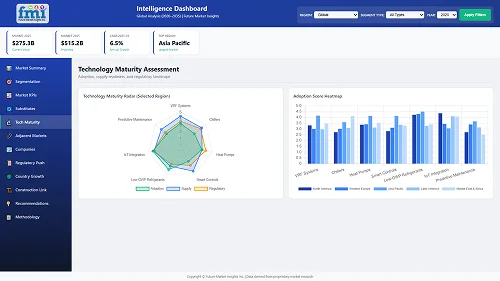
Market Position: Employee benefits TPA systems command the leading position in the Third Party Administration (TPA) Service market with approximately 48.0% market share through advanced administrative capabilities, including superior enrollment processing, comprehensive benefit management, and cost optimization that enable organizations to achieve optimal workforce satisfaction across diverse corporate and insurance environments.
Value Drivers: The segment benefits from employer preference for reliable administrative systems that provide consistent processing performance, reduced overhead costs, and employee satisfaction without requiring significant internal resource allocation. Advanced service features enable automated enrollment systems, benefits coordination, and integration with existing HR platforms, where processing accuracy and compliance reliability represent critical operational requirements.
Competitive Advantages: Employee benefits TPA systems differentiate through proven regulatory compliance, consistent processing quality, and integration with payroll systems that enhance operational effectiveness while maintaining optimal accuracy suitable for diverse corporate applications.
Key market characteristics:
Healthcare TPA systems maintain specialized service positioning in the Third Party Administration (TPA) Service market due to their medical expertise and clinical processing advantages. These systems appeal to organizations requiring specialized administrative capabilities with comprehensive performance for medical claims processing applications. Market adoption is driven by healthcare complexity expansion, emphasizing accurate claims adjudication and operational efficiency through optimized medical review systems while maintaining regulatory compliance structures.
-service-market-analysis-by-application.webp)
Market Context: Healthcare industry applications dominate the Third Party Administration (TPA) Service market with approximately 40.0% market share due to widespread adoption of outsourced administration and increasing focus on claims processing efficiency, cost management, and regulatory compliance applications that minimize processing errors while maintaining industry standards.
Appeal Factors: Healthcare organizations prioritize processing reliability, regulatory consistency, and integration with existing provider infrastructure that enables coordinated administrative services across multiple benefit programs. The segment benefits from substantial healthcare industry investment and cost reduction programs that emphasize the acquisition of TPA services for claims management and compliance applications.
Growth Drivers: Healthcare cost containment programs incorporate TPA services as standard administration for medical claims operations, while insurance industry growth increases demand for processing capabilities that comply with regulatory standards and minimize administrative overhead.
Market Challenges: Varying healthcare regulations and medical claim complexity differences may limit administrative standardization across different provider networks or operational scenarios.
Application dynamics include:
Insurance industry applications capture approximately 35.0% market share through specialized administrative requirements in policy management, claims adjudication, and multi-carrier coordination applications. These organizations demand robust TPA systems capable of managing complex benefit structures while providing comprehensive compliance and efficient processing capabilities.
Construction and real estate industry applications account for approximately 12.0% market share, transportation industry captures 8.0%, while other segments represent 5.0%, including workers' compensation administration, specialized employee benefits, and niche risk management applications requiring TPA capabilities for regulatory compliance and cost optimization.
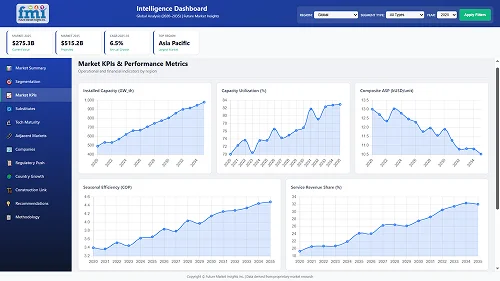
Growth Accelerators: Corporate cost reduction drives primary adoption as TPA services provide superior administrative efficiency that enables employers to meet regulatory compliance standards without excessive overhead costs, supporting benefit operations and employee satisfaction missions that require precise claims processing applications. Healthcare complexity management demand accelerates market expansion as insurance carriers seek effective outsourcing systems that minimize errors while maintaining operational effectiveness during enrollment and claims adjudication scenarios. Corporate benefits spending increases worldwide, creating sustained demand for administrative systems that complement traditional HR processes and provide cost optimization in competitive labor markets.
Growth Inhibitors: Data security cost challenges vary across TPA providers regarding the protection of sensitive health information and compliance with privacy regulations, which may limit operational flexibility and market penetration in regions with stringent data protection requirements or security-sensitive organizations. Technical performance limitations persist regarding legacy system integration and platform compatibility concerns that may reduce effectiveness in complex multi-carrier environments, technology transitions, or enterprise-wide implementations, affecting processing efficiency and service requirements. Market fragmentation across multiple regulatory standards and benefit plan designs creates compatibility concerns between different TPA providers and existing administrative infrastructure.
Market Evolution Patterns: Adoption accelerates in healthcare and insurance sectors where administrative complexity justifies outsourcing costs, with geographic concentration in developed markets transitioning toward mainstream adoption in emerging economies driven by healthcare expansion and regulatory awareness. Technology development focuses on enhanced processing automation, improved compliance integration, and compatibility with cloud-based systems that optimize claims accuracy and administrative effectiveness. The market could face disruption if artificial intelligence technologies or blockchain innovations significantly limit the deployment of traditional TPA services in benefit administration applications, though TPA services' unique combination of regulatory expertise, processing accuracy, and cost efficiency continues to make them preferred in healthcare applications.
The Third Party Administration (TPA) Service market demonstrates varied regional dynamics with Growth Leaders including China (5.3% CAGR) and India (4.9% CAGR) driving expansion through healthcare capacity additions and insurance modernization programs. Steady Performers encompass Germany (4.5% CAGR), Brazil (4.1% CAGR), USA (3.7% CAGR), UK (3.3% CAGR), and Japan (2.9% CAGR), benefiting from established healthcare industries and advanced outsourcing adoption.
-service-market-cagr-analysis-by-country.webp)
| Country | CAGR (2025-2035) |
|---|---|
| China | 5.3% |
| India | 4.9% |
| Germany | 4.5% |
| Brazil | 4.1% |
| USA | 3.7% |
| UK | 3.3% |
| Japan | 2.9% |
Regional synthesis reveals Asia Pacific markets leading adoption through healthcare infrastructure expansion and insurance industry development, while European countries maintain steady expansion supported by administrative outsourcing advancement and regulatory standardization requirements. North American markets show moderate growth driven by corporate benefits applications and healthcare cost management trends.
-service-market-country-value-analysis.webp)
The Chinese market emphasizes advanced administrative features, including precision claims processing and integration with comprehensive healthcare platforms that manage benefit quality, compliance optimization, and cost control applications through unified monitoring systems. The country demonstrates strong growth at 5.3% CAGR, driven by healthcare insurance expansion, employee benefits initiatives, and emerging corporate benefit development that support TPA service integration. Chinese insurance organizations prioritize operational effectiveness with TPA services delivering consistent processing accuracy through advanced technology capabilities and regulatory adaptation features.
Technology deployment channels include major insurance carriers, specialized TPA providers, and corporate procurement programs that support professional applications for complex healthcare administration and benefit management applications. Platform integration capabilities with established insurance systems expand market appeal across diverse operational requirements seeking cost efficiency and compliance benefits. The expanding middle-class workforce and accelerating health insurance market create sustained demand, while innovative applications in digital health platforms and wellness programs open new growth avenues.
Performance Metrics:
Germany's advanced healthcare market demonstrates sophisticated TPA deployment with documented operational effectiveness in employee benefits administration and insurance claims facilities through integration with existing administrative systems and regulatory infrastructure. The country leverages engineering expertise in compliance management and systems integration to maintain strong growth at 4.5% CAGR. Industrial centers, including Frankfurt, Munich, and Hamburg, showcase premium installations where TPA systems integrate with comprehensive healthcare platforms and benefits management systems to optimize insurance operations and administrative effectiveness.
German TPA providers prioritize regulatory compliance and EU standards in service development, creating demand for premium administrative systems with advanced features, including GDPR integration and automated processing systems. The market benefits from established insurance infrastructure and a willingness to invest in outsourcing technologies that provide long-term cost benefits and compliance with international data protection and quality standards.
Market Intelligence Brief:
The USA TPA service market demonstrates sophisticated deployment across healthcare applications with documented effectiveness in employee benefits administration and insurance claims facilities through integration with comprehensive compliance management systems and regulatory infrastructure. The country leverages advanced technology capabilities in platform innovation and processing automation to maintain moderate growth at 3.7% CAGR. Industrial centers, including New York, Chicago, and Dallas, showcase premium installations where TPA systems integrate with comprehensive healthcare platforms and corporate benefit networks to optimize cost management and administrative effectiveness.
American employers prioritize cost reduction and service quality in administrative development, creating demand for innovative TPA systems with advanced features, including artificial intelligence integration and automated claims systems. The market benefits from established healthcare infrastructure and willingness to invest in outsourcing technologies that provide long-term efficiency benefits and compliance with HIPAA and regulatory standards.
Market Intelligence Brief:
The UK TPA service market demonstrates advanced compliance deployment with documented operational effectiveness in insurance administration applications and corporate benefits facilities through integration with existing regulatory systems and administrative infrastructure. The country leverages regulatory expertise in data protection and systems integration to maintain steady growth at 3.3% CAGR. Industrial centers, including London, Manchester, and Birmingham, showcase premium installations where TPA systems integrate with comprehensive compliance platforms and benefits management systems to optimize regulatory adherence and administrative effectiveness.
British employers prioritize data protection and regulatory compliance in service development, creating demand for certified TPA systems with advanced features, including privacy safeguards and audit trail integration. The market benefits from established insurance infrastructure and commitment to invest in outsourcing technologies that provide long-term compliance benefits and adherence with UK and EU data protection standards. Healthcare administration applications, insurance processing systems, and corporate benefit programs drive diversified demand across multiple end-use segments.
Strategic Market Indicators:
India's TPA service market demonstrates rapid expansion deployment with documented operational effectiveness in healthcare insurance applications and corporate benefits facilities through integration with emerging insurance systems and benefit development infrastructure. The country leverages growing service capabilities in administrative processing and systems integration to achieve high growth at 4.9% CAGR. Industrial centers, including Mumbai, Delhi, and Bangalore, showcase expanding installations where TPA systems integrate with comprehensive insurance platforms and corporate networks to optimize market penetration and administrative effectiveness.
Indian insurance organizations prioritize cost efficiency and service quality in administrative development, creating demand for sophisticated TPA systems with advanced features, including automated processing integration and compliance control systems. The market benefits from expanding healthcare infrastructure and willingness to invest in international-standard administrative technologies that provide cost optimization and compliance with evolving regulatory standards.
Market Intelligence Brief:
Brazil's TPA service market demonstrates growth deployment with documented operational effectiveness in health insurance applications and corporate benefits facilities through integration with expanding insurance systems and healthcare infrastructure. The country leverages economic capabilities in insurance growth and administrative systems integration to maintain steady growth at 4.1% CAGR. Industrial centers, including Sao Paulo, Rio de Janeiro, and Belo Horizonte, showcase expanding installations where TPA systems integrate with comprehensive insurance platforms and employer networks to optimize cost management and administrative effectiveness.
Brazilian employers prioritize administrative efficiency and regulatory compliance in service development, creating demand for cost-effective TPA systems with advanced features, including local regulatory adaptation and claims processing systems. The market benefits from growing healthcare infrastructure and commitment to invest in outsourcing technologies that provide cost optimization and compliance with Brazilian healthcare standards.
Strategic Market Indicators:
Japan's TPA service market demonstrates precision deployment with documented operational effectiveness in premium healthcare administration and corporate benefits facilities through integration with advanced insurance systems and quality control infrastructure. The country leverages service excellence in administrative processing and systems integration to maintain steady growth at 2.9% CAGR. Industrial centers, including Tokyo, Osaka, and Yokohama, showcase premium installations where TPA systems integrate with comprehensive quality platforms and compliance systems to optimize service excellence and administrative effectiveness.
Japanese employers prioritize processing precision and service quality in administrative development, creating demand for ultra-premium TPA systems with advanced features, including micro-precision processing and quality integration systems. The market benefits from established insurance infrastructure and commitment to invest in highest-quality administrative technologies that provide superior accuracy and compliance with stringent Japanese regulatory standards.
Strategic Market Indicators:
-service-market-europe-country-market-share-analysis,-2025-&-2035.webp)
The Third Party Administration (TPA) Service market in Europe is projected to grow from USD 2.7 billion in 2025 to USD 3.7 billion by 2035, registering a CAGR of 3.2% over the forecast period. Germany is expected to maintain its leadership position with a 29.4% market share in 2025, declining slightly to 28.7% by 2035, supported by its advanced insurance infrastructure and major administrative service centers in Frankfurt and Munich. The UK follows with a 21.6% share in 2025, projected to reach 21.9% by 2035, driven by comprehensive healthcare outsourcing programs and regulatory compliance initiatives.
France holds a 16.8% share in 2025, expected to increase to 17.2% by 2035 through steady insurance modernization activities. Italy commands a 13.5% share, while Spain accounts for 9.2% in 2025. The Rest of Europe region is anticipated to show steady adoption, expanding its collective share from 9.5% to 10.3% by 2035, reflecting consistent growth in Nordic countries, insurance expansion in Central European markets, and administrative outsourcing upgrades across Eastern European healthcare facilities.
-service-market-japan-market-share-analysis-by-service-type.webp)
In Japan, the Third Party Administration (TPA) Service market prioritizes employee benefits TPA systems, which capture the dominant share of corporate and insurance installations due to their advanced features, including precision processing optimization and seamless integration with existing HR infrastructure. Japanese employers emphasize reliability, precision, and long-term compliance excellence, creating demand for employee benefits TPA systems that provide consistent administrative capabilities and superior service performance based on regulatory requirements and quality standards.
Healthcare TPA maintains secondary positions primarily in specialized medical claims applications and provider network installations where comprehensive administrative functionality meets operational requirements without compromising processing efficiency.
Market Characteristics:
-service-market-south-korea-market-share-analysis-by-application.webp)
In South Korea, the market structure favors international TPA providers, including Public Consulting Group, Andesa, and BRMS, which maintain dominant positions through comprehensive service portfolios and established insurance industry networks supporting both employee benefits administration and healthcare claims processing installations.
These providers offer integrated solutions combining advanced TPA systems with professional consulting services and ongoing compliance support that appeal to Korean employers seeking reliable administrative outsourcing systems. Local administrative service contractors and benefits consultants capture moderate market share by providing localized service capabilities and competitive pricing for standard benefit administration installations, while domestic providers focus on specialized applications and cost-effective solutions tailored to Korean healthcare market characteristics.
Channel Insights:
-service-market-analysis-by-company.webp)
The Third Party Administration (TPA) Service market operates with moderate concentration, featuring approximately 18-24 meaningful participants, where leading companies control roughly 38-44% of the global market share through established insurance industry relationships and comprehensive service portfolios. Competition emphasizes advanced processing capabilities, regulatory compliance, and technology integration rather than price-based rivalry. The leading company, Public Consulting Group, commands approximately 14% market share through its extensive administrative service line and global healthcare industry presence.
Market Leaders encompass Public Consulting Group, Andesa, and BRMS, which maintain competitive advantages through extensive administrative expertise, global insurance carrier networks, and comprehensive technology integration capabilities that create customer loyalty and support premium pricing. These companies leverage decades of benefits administration experience and ongoing technology investments to develop advanced TPA systems with precision compliance control and automation features. Technology Innovators include TRM and regional specialists, which compete through specialized processing technology focus and innovative compliance capabilities that appeal to employers seeking advanced administrative solutions and cost optimization.
These companies differentiate through rapid technology development cycles and specialized healthcare application focus. Regional Specialists feature TPA providers focusing on specific geographic markets and specialized applications, including regulatory compliance systems and integrated insurance carrier solutions. Market dynamics favor participants that combine reliable administrative platforms with advanced processing capabilities, including precision compliance control and automatic accuracy optimization features. Competitive pressure intensifies as traditional insurance carriers expand into TPA services, while specialized healthcare technology companies challenge established players through innovative processing solutions and cloud-based platforms targeting employee benefits and healthcare claims segments.
| Item | Value |
|---|---|
| Quantitative Units | USD 9.6 billion |
| Service Type | Employee Benefits TPA, Healthcare TPA, Pension TPA, Risk Management TPA, Others |
| Application | Healthcare Industry, Insurance Industry, Construction and Real Estate Industry, Transportation Industry, Others |
| Regions Covered | Asia Pacific, Europe, North America, Latin America, Middle East & Africa |
| Countries Covered | China, India, Germany, Brazil, USA, UK, Japan, and 20+ additional countries |
| Key Companies Profiled | Public Consulting Group, Andesa, BRMS, TRM, UMR, Crawford & Company, UMP, CorVel, Meritain Health, ESIS, Helmsman Management Services, HealthSmart, Gallagher Bassett, Personify Health, Careington Benefit Solutions, Allegiance, Anthem, Burnham & Flower, HealthEZ, Medilin, Raffles Health Insurance, McLarens, EXL, Brighton Health Plan Solutions |
| Additional Attributes | Dollar sales by service type and application categories, regional adoption trends across Asia Pacific, Europe, and North America, competitive landscape with TPA providers and insurance carrier suppliers, employer preferences for cost efficiency and regulatory compliance, integration with healthcare platforms and benefits monitoring systems, innovations in automated processing solutions and compliance excellence, and development of cloud-based administrative solutions with enhanced performance and cost optimization capabilities. |
The global third party administration (TPA) service market is estimated to be valued at USD 9.6 billion in 2025.
The market size for the third party administration (TPA) service market is projected to reach USD 14.1 billion by 2035.
The third party administration (TPA) service market is expected to grow at a 3.9% CAGR between 2025 and 2035.
The key product types in third party administration (TPA) service market are employee benefits tpa, healthcare tpa, pension tpa, risk management tpa and others.
In terms of application, healthcare industry segment to command 40.0% share in the third party administration (TPA) service market in 2025.
Full Research Suite comprises of:
Market outlook & trends analysis
Interviews & case studies
Strategic recommendations
Vendor profiles & capabilities analysis
5-year forecasts
8 regions and 60+ country-level data splits
Market segment data splits
12 months of continuous data updates
DELIVERED AS:
PDF EXCEL ONLINE
Third-Party Risk Management Market Size and Share Forecast Outlook 2025 to 2035
Third Party Logistics Services Market Size and Share Forecast Outlook 2025 to 2035
Fourth Party Logistics Market Size and Share Forecast Outlook 2025 to 2035
Postpartum Health Supplements Market Size and Share Forecast Outlook 2025 to 2035
Postpartum Depression Management Market Size and Share Forecast Outlook 2025 to 2035
Outpatient Clinics Market Trends and Forecast 2025 to 2035
MFTPaaS Market
Service Lifecycle Management Application Market Size and Share Forecast Outlook 2025 to 2035
Service Delivery Automation Market Size and Share Forecast Outlook 2025 to 2035
ServiceNow Tech Service Market Size and Share Forecast Outlook 2025 to 2035
Service Orchestration Market Size and Share Forecast Outlook 2025 to 2035
Service Robotics Market Size and Share Forecast Outlook 2025 to 2035
Service Trucks Market Size and Share Forecast Outlook 2025 to 2035
Service Resource Planning (SRP) SaaS Solutions Market Size and Share Forecast Outlook 2025 to 2035
Service Bureau Market Analysis - Size, Growth, and Forecast 2025 to 2035
Service Laboratory Market Analysis by Service Type, Deployment, Channel, End-user, and Region Through 2035
Service Integration & Management Market Report – Forecast 2017-2027
IT Service Management Tools Market Growth – Trends & Forecast through 2034
M2M Services Market Size and Share Forecast Outlook 2025 to 2035
Foodservice Equipment Market Analysis - Size, Share, and Forecast Outlook 2025 to 2035
Thank you!
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.
Chat With
MaRIA